Chemistry Team Outwits Drug-Resistant Lung Bacteria Using Nanotech and Nitric Oxide
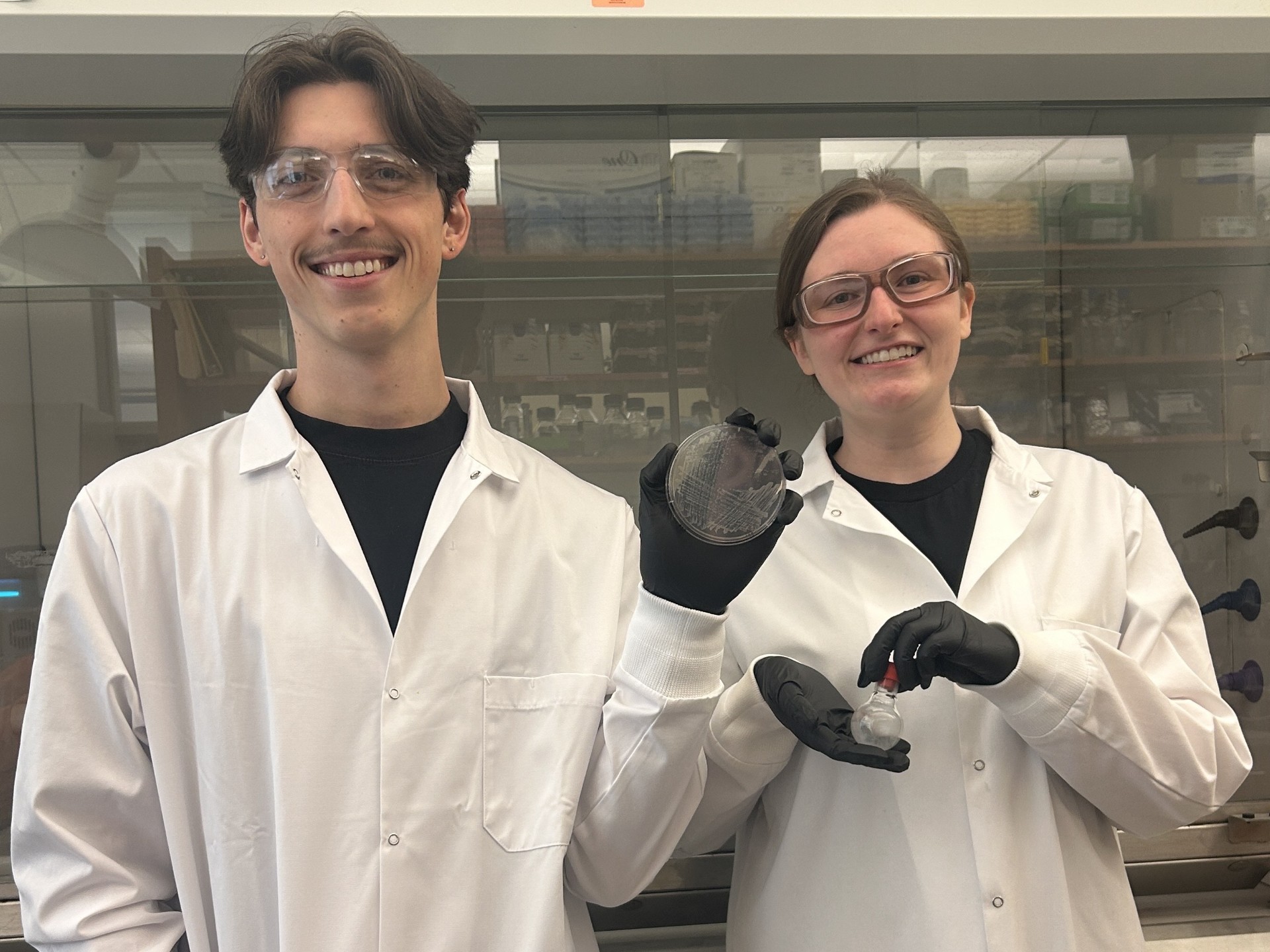
UNC chemistry Ph.D. students Sarah Nagy, right, and Joseph Metiva, under the guidance of Dr. Mark Schoenfisch, the Peter A. Ornstein Distinguished Professor of Chemistry, have created a better way to deliver nitric oxide into infected lung cells where antibiotics often can’t reach.
June 10, 2025 I By Dave DeFusco
In a lab at UNC-Chapel Hill, a team of chemists is tackling one of the toughest bacterial infections facing patients with lung disease—Mycobacterium abscessus, a fast-growing and drug-resistant germ that can turn deadly. Their solution is tiny vehicles packed with a molecule the body already makes—nitric oxide.
The study, published in the journal ACS Applied Bio Materials, was led by UNC chemistry Ph.D. students Sarah Nagy and Joseph Metiva under the guidance of Dr. Mark Schoenfisch, the Peter A. Ornstein Distinguished Professor of Chemistry. Their goal: to create a better way to deliver nitric oxide into infected cells, where antibiotics often can’t reach.
“This bacterium is notoriously hard to treat,” said Nagy. “It grows quickly, survives inside cells and resists almost every antibiotic we throw at it.”
Nontuberculous mycobacteria (NTM), like M. abscessus, are found in soil, water and dust. For most people, they pose little risk. But in older adults or people with weakened immune systems, these bacteria can cause chronic lung infections. Once they take hold, they’re incredibly hard to eliminate.
 Patients often spend years on a grueling regimen of multiple antibiotics—with serious side effects. Even then, the success rate of eradicating the infection is low. What makes M. abscessus especially troublesome is its ability to hide inside cells and form biofilms, which help it evade both the immune system and drugs.
Patients often spend years on a grueling regimen of multiple antibiotics—with serious side effects. Even then, the success rate of eradicating the infection is low. What makes M. abscessus especially troublesome is its ability to hide inside cells and form biofilms, which help it evade both the immune system and drugs.
“Standard antibiotics aren’t designed to get inside human cells,” said Metiva. “That’s a huge problem, because this bacterium sets up shop inside the very cells that are supposed to kill it.”
That’s where nitric oxide, or NO, comes in. It’s a free radical that the human body naturally produces to help regulate blood flow, fight off infections and signal between cells. Scientists have known for years that NO can kill bacteria, but delivering it in a safe and effective way has been a major hurdle.

Directly inhaling nitric oxide gas hasn’t worked well. Too little and it’s ineffective, too much and it’s toxic. But the UNC team used a NO donor compound called MD3, a specially designed molecule that slowly releases nitric oxide over time. The problem is that MD3 is highly charged, which makes it difficult for it to get into cells on its own.
So the researchers put MD3 into liposomes—microscopic spheres made of lipids, similar to the membranes of human cells. Liposomes can pass through cell membranes and release their contents inside. Think of them as tiny Trojan horses, delivering a payload of a bacteria-killing molecule where it’s needed most.
“By using liposomes, we were able to sneak the NO donor inside infected cells,” said Nagy. “Once inside, it releases a large nitric oxide payload directly onto the bacteria.”
The team tested their liposomal nitric oxide system on two versions of M. abscessus—a “smooth” version that hides from the immune system and a “rough” one that causes more inflammation and damage. Both are common in patients and difficult to treat.
The results were striking: The liposomal formulation significantly outperformed non-liposomal MD3 in preventing and breaking down bacterial biofilms. At higher doses, it completely killed the bacteria within the biofilms—a crucial achievement, since biofilms are notoriously hard to treat. Even more promising, the treatment worked inside infected cells, reducing the number of bacteria by almost 100%—a 1,000-fold drop— at concentrations lung tissues can tolerate.
“What was really exciting,” said Metiva, “was seeing how much more our cargo got inside the cells when we used liposomes. It was more than three times as much compared to our control.”
The research is still in early stages and has only been tested in cell cultures, not yet in animals or humans. But the team is hopeful that their work will lay the groundwork for new treatments—not just for M. abscessus, but potentially for other hard-to-treat infections as well. Dr. Schoenfisch, who has spent two decades studying nitric oxide, emphasized the broader significance of the findings.
“This study demonstrates that we can overcome two of the biggest challenges in treating intracellular infections: drug delivery and resistance,” he said. “By using nitric oxide instead of antibiotics, we’re hitting bacteria in ways they can’t easily defend against. And by using liposomes, we’re getting the molecule to where it needs to go.”