Chemistry Alum Helps Revive an Old Anesthetic for Modern Emergencies
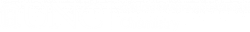
Katelyn Kitzinger, who earned a Ph.D. in organic chemistry, holds aloft a 3D molecular model of diethyl ether, a 19th-century chemical that was once the world’s most common anesthetic. She joined a team of UNC researchers in chemistry and medicine to explore an unexpected question: Could doctors make their own anesthetic in the field using simple materials?
October 27, 2025 | By Dave DeFusco
When earthquakes, wars or hurricanes devastate communities, hospitals can disappear overnight. Doctors may have no electricity, few medicines and no safe way to put patients to sleep for surgery. In those moments, something as routine as an appendectomy can become impossible.
That urgent problem led Katelyn Kitzinger, who holds a Ph.D. in organic chemistry from UNC-Chapel Hill, to join a team exploring an unexpected question: Could doctors make their own anesthetic in the field using simple materials? The answer, she and her colleagues found, might lie in a 19th-century chemical called diethyl ether, once the world’s most common anesthetic. Ether was replaced long ago by safer, less flammable drugs, but it has two big advantages in a crisis: it works and it’s easy to make.

“It’s one of the simplest anesthetics ever used,” said Kitzinger, now a senior scientist at AbbVie, a global pharmaceutical company. “Chemically, it’s made from alcohol. If you can produce it safely, it could be a lifesaver where modern anesthetics just can’t reach.”
Her study, “Is Small-scale Production of Diethyl Ether for Anesthetic Use Possible?” published in the Journal of Special Operations Medicine, set out to prove that point with the design of a small-scale experiment using materials that might be available in almost any country.
A key figure behind the project was Sandeep Dhanjal, an assistant professor of anesthesiology in the UNC School of Medicine who focuses on global health. He approached Kitzinger and Jeffrey Johnson, A. Ronald Gallant Distinguished Professor, with a pressing question: how could doctors in resource-limited or disaster-stricken settings safely produce anesthetics when commercial supplies were unavailable?
Acting as both the catalyst and clinical partner, Dhanjal worked closely with Kitzinger to run the experiments after Johnson’s group explored the chemical feasibility. Their collaboration became the project’s defining strength, showing how people from very different parts of the university could combine their expertise to tackle a real-world humanitarian challenge.

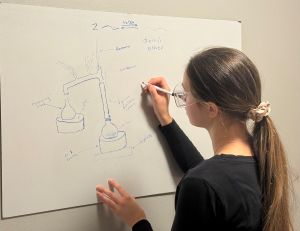
The idea was straightforward: start with ethanol—the same type of alcohol found in hand sanitizer or spirits—and add sulfuric acid, a common chemical that’s found in some household drain cleaners. Heat the mixture to about 145 degrees Celsius, or 290 degrees Fahrenheit, and a chemical reaction occurs that transforms some of the alcohol into diethyl ether and water.
The next challenge was to separate and purify the ether so that it could be safely used as an anesthetic. “The tricky part is that diethyl ether evaporates very quickly,” said Kitzinger. “If you leave it sitting out, it’ll be gone in minutes.”
To keep it from disappearing, the team used a simple setup: a glass flask connected to a cooling tube that collected the ether vapors into a second container chilled in an ice bath. “That’s how we kept it from escaping,” she said. “It’s not high-tech. You could imagine doing something similar in a basic lab setup.”
When the team analyzed what they’d made, they found that the sample was 97% pure ether, with the remaining 3% being leftover ethanol. “We were happy to see that the impurity was just ethanol,” said Kitzinger. “It’s something that’s already safe for the body, so we weren’t introducing anything dangerous.”
To confirm what they had made, Kitzinger used a tool called proton nuclear magnetic resonance spectroscopy, or proton NMR. This method works a bit like fingerprinting; it produces a unique pattern for each chemical. “Every molecule has its own signature,” she said. “When we saw the pattern for ether, we knew exactly what we had.”
Still, ether’s flammability poses a real risk, especially in field conditions. Kitzinger said the way to minimize that danger is by keeping the apparatus sealed, cooling the collection container and avoiding open flames. “It’s about containment,” she said. “If you can prevent vapors from getting into the air, you greatly reduce the fire hazard.”
In brainstorming sessions, the team even discussed whether doctors could use cheap vodka as the alcohol source or drain cleaner as the acid catalyst. “We were thinking, how do you make this as practical as possible?” said Kitzinger. “Of course, safety is the top priority, but it’s interesting to think about how you could adapt chemistry to real-world constraints.”
For Kitzinger, the project was a reminder of why she became a scientist. “It was really exciting to take something I learned in an undergraduate chemistry class and use it to address a humanitarian problem,” she said. “I got into science because I wanted to make a positive impact, and this felt like one of those rare projects that connects chemistry directly to helping people.”
She credits Johnson, her graduate mentor, with nurturing that mindset. “He was a great example of what it means to be a good scientist—curious, encouraging and willing to take on tough questions,” she said. “He gave me the freedom to explore new ideas, even if they seemed a little unconventional.”
Today, Kitzinger applies that same curiosity and approach to problem-solving in AbbVie’s process chemistry department, where her team develops large-scale synthetic routes for chemicals of pharmaceutical importance. Their focus is on making these reactions safe, efficient and reproducible while ensuring the highest product purity. To do that, they rely on a wide range of analytical tools and reaction-monitoring techniques.
“Scaling up a reaction, from a small vial in the lab to a large reactor in a manufacturing plant, can change its behavior in surprising ways,” said Kitzinger, “and part of my job is figuring out why. Understanding how molecules transform from starting materials to final products is critical, and we build that knowledge through both experimental work and insights drawn from the scientific literature.”
As for the future of ether production in crisis medicine, Kitzinger hopes others will build on her proof-of-concept study to test safer equipment, find better starting materials and develop simple field tests to confirm the quality of the ether produced.
“If we could come up with a way for doctors to verify what they made without fancy lab equipment, that would be huge,” she said. “It could make surgery possible in places where it currently isn’t. Sometimes the solutions we need are already in the past. We just have to look at them with fresh eyes.”